

A 28-Year-Old Woman With Severe Headaches
Jul 12-00
Rohit Bakshi, MD
[Medscape Neurology, 2000. © 2000 Medscape, Inc.]
Case Presentation
A 28-year-old woman presents to the emergency room with the worst
headache of her life. Her medical history is unremarkable except for a
several-year history of mild occasional headaches that respond to analgesics.
However, 2 weeks ago, she developed a different type of headache that was
much more severe and occurred daily. Noncontrast CT of the brain is
performed. The representative images are shown in Figure 1.

Figure 1. This is a Noncontrast CT scan of the
brain. Representative axial slices are shown at the level of the
third ventricle (left) and lateral ventricular bodies (right).
Question 1. CT imaging relies on:
A: Nonionizing radiation
B: Radiofrequency pulses
C: Differences in tissue attenuation of x-ray beams
D: Uptake of radiotracers by cells
E: Passage of air into the cerebrospinal fluid
Question 2. The units of measure of the data generated by CT are:
A: Roentgen units
B: Oldendorf units
C: Larmor units
D: Mazziotta units
E: Hounsfield units
Question 3. Which of the following is an advantage of CT over MRI?
A: Not affected by beam hardening artifact
B: Lack of ionizing radiation
C: Safer in pregnancy
D: Sensitivity for white matter disease
E: Visualization of bony lesions
Question 4. Which is true of the findings in Figure 1?
A: Diffuse cerebral edema
B: Subarachnoid hemorrhage
C: Subdural hemorrhage
D: Cerebral venous thrombosis
E: Normal findings
------------------------- ooooooooo -----------------------------
Answers
1.C. CT scanning is based on differences in tissue attenuation of x-ray beams
2.E. Hounsfield units, a measure of tissue density, are obtained by CT.
3.E. CT is currently superior to MRI in the detection of lesions in cortical bone.
4.D. The CT findings in this case are suspicious for cerebral venous thrombosis.
The following questions are based on Figure 2, which shows the same images as
figure 1 with arrows added for illustrative purposes.
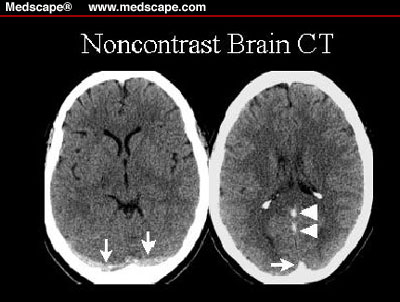
Figure 2. The same CT images from Figure 1. Arrows are placed on the scans to illustrate the
abnormal findings as described in the text.
Question 5. The hyperdensities (arrows) on the left CT scan are indicative of thrombosis in:
A:Cortical veins
B:Vein of Labbé
C:Transverse sinuses
D:Deep cerebral venous system
E:The torcula herophili
Question 6. The arrowheads in the right CT scan point to hyperdensities that are indicative of thrombosis in:
A:Inferior sagittal sinus
B:Superior sagittal sinus
C:Vein of Labbé
D:Vein of Galen and straight sinus
E:Basal vein of Rosenthal
Question 7. The arrow in the right CT scan points to hyperdensity that is indicative of thrombosis in:
A:Inferior sagittal sinus
B:Superior sagittal sinus (torcula herophili)
C:Vein of Labbé
D:Vein of Galen and straight sinus
E:Basal vein of Rosenthal
--------------- OOOOOOOOOO -------------------
Answers
5.C. The hyperdensities (arrows) on the left CT scan are indicative of thrombosis in the transverse sinuses bilaterally.
6.D. The arrowheads in the right CT scan point to hyperdensities that are indicative of thrombosis in the deep venous system, including the straight sinus and the vein of Galen.
7.B. The arrow in the right CT scan points to hyperdensity that is indicative of thrombosis in the superior sagittal sinus as it joins the confluence of sinuses (torcula herophili).
MRI, MR venography, and conventional angiography of this patient were
consistent with cerebral venous thrombosis (CVT). The patient's only identified risk factor was the use of oral contraceptive agents.
She responded well to heparinization, IV hydration, and short-term oral warfarin anticoagulation.
Discussion
The causes of CVT include pregnancy, collagen vascular disorders,
inflammatory bowel disease, and hypercoagulable states as well as local
processes such as infection, neoplastic disease, trauma, and medications such as
lithium.[1-5] CVT begins with progressive venous occlusion followed by
collateralization and recanalization. If collateralization is inadequate, venous
occlusion may lead to congestion resulting in parenchymal injury and
hemorrhage (venous stroke). CVT may present with indolent symptoms over
weeks to months or with acute catastrophic neurologic sequelae. The presenting
symptoms may include headache, seizures, and/or focal neurologic dysfunction,
but these findings are nonspecific.[2,4] CVT may be difficult to diagnose on
clinical grounds alone.[4] Early diagnosis of CVT is important because of the high
morbidity associated with it[4] and the possibility to successfully treat this
condition with anticoagulation[4] or local thrombolytic therapy.[5] A recent
retrospective study comparing local urokinase thrombolysis to heparin therapy
for CVT suggests that thrombolysis treatment leads to a better neurologic
recovery,[6] thus warranting a prospective randomized trial comparing urokinase
thrombolysis with heparin anticoagulation.
CT findings in CVT may be subtle, especially if venous stroke has not occurred.
Because of the proximity of venous sinuses to cranial bone and dura, the
hyperdensities of the thrombosis may be inconspicuous.
MRI has improved the diagnosis of CVT and associated stroke and
hemorrhage.[1,2,4,7,8] Venous strokes do not conform to arterial territories; they
are frequently bilateral and hemorrhagic. Venous strokes may show
parenchymal contrast enhancement and extensive mass effect on MRI, therefore
resembling tumors.[2] The diagnosis of CVT relies on the depiction of blood
clots in the venous system on MRI scans or altered venous flow on MR
venograms. MRI findings include loss of the normal venous flow void, lack of
normal venous enhancement, and visualization of signal changes in the venous
channels on T1 and T2 images. 3-D phase contrast MR venography (sensitive
to slow flow) is the preferred MR method to confirm the diagnosis of CVT.

--------- end ----------------
Para volver a la primera pagina:-HAGA CLIC AQUI